-
Tips for becoming a good boxer - November 6, 2020
-
7 expert tips for making your hens night a memorable one - November 6, 2020
-
5 reasons to host your Christmas party on a cruise boat - November 6, 2020
-
What to do when you’re charged with a crime - November 6, 2020
-
Should you get one or multiple dogs? Here’s all you need to know - November 3, 2020
-
A Guide: How to Build Your Very Own Magic Mirror - February 14, 2019
-
Our Top Inspirational Baseball Stars - November 24, 2018
-
Five Tech Tools That Will Help You Turn Your Blog into a Business - November 24, 2018
-
How to Indulge on Vacation without Expanding Your Waist - November 9, 2018
-
5 Strategies for Businesses to Appeal to Today’s Increasingly Mobile-Crazed Customers - November 9, 2018
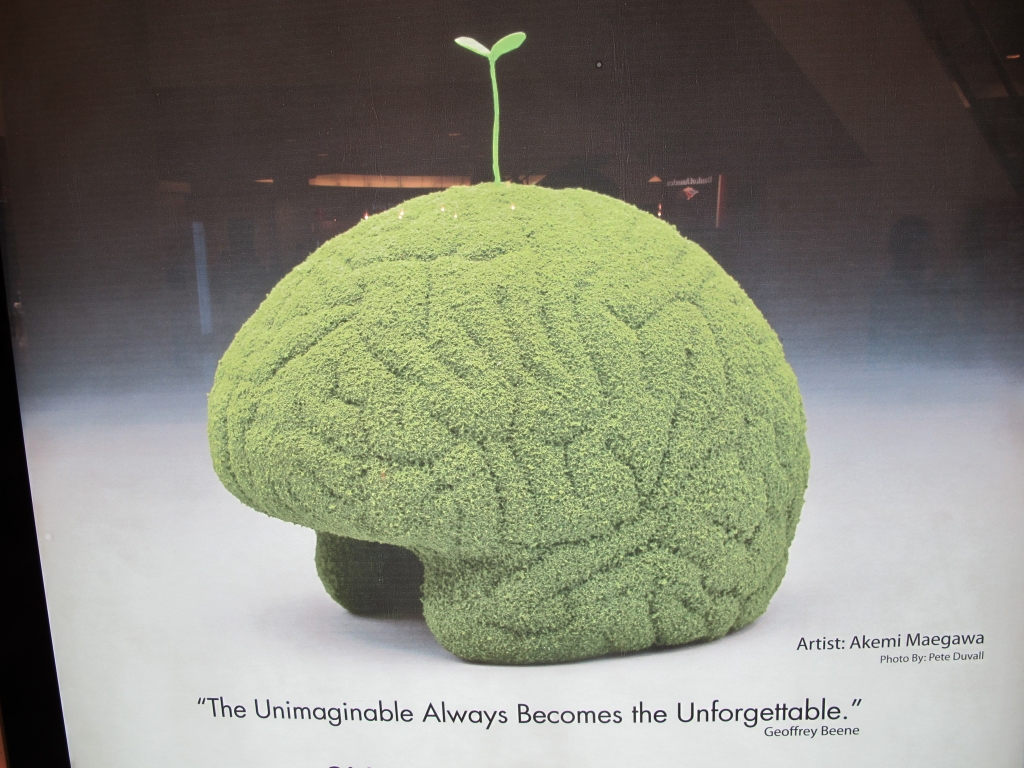
Alzheimer’s disease protein link with brain stress response found
The research was conducted on mouse models as well as in human cells. They discovered that stress-coping hormones released by the brain produce amyloid beta fragments that clump together and increase the risk of degeneration in the brain.
Advertisement
This is not the first scientific project to link the two to one another, however it is the first to offer any proof of the mechanics through witch stress may lead to the disease.
Prof Golde, of the University of Florida, said: “It adds detailed insight into the stress mechanisms that might promote at least one of the Alzheimer’s pathologies”. Their plan is to use an antibody known for blocking the release of the stress hormone in order to inhibit the production of the protein associated with Alzheimer’s.
The study found stress releases a hormone called CRF (corticotrophin releasing factor) in the brain which, in turn, increases production of amyloid beta.
According to official stats, more than 5 million Americans are living with Alzheimer’s (AD) at present.
Prof Golde said: “These softer, non genetic factors that may confer risk of Alzheimer’s disease are much harder to address”.
Ahead of World Alzheimer’s Day, scientists have announced a breakthrough in removing amyloid-beta from the brain. However, researchers are increasingly linking stress to onset of the disease.
Working with the Dublin Brain Bank, which is based in Beaumont Hospital, the researchers from Trinity examined brain tissues of individuals who were affected by Alzheimer’s disease during their lifetime and then compared results to those observed in model systems in the laboratory. The stress hormone, CRF, causes an enzyme known as gamma secretase to increase its activity. The researchers used extensive neuroimaging which included volumetric MRI, FDG PET, amyloid PET and retinal amyloid imaging to quantify the amount of amyloid that was present in the brain of the patients at various stages of the study. However, the researchers admit this approach will be challenging. “By studying these individuals, we can develop insights into how Alzheimer’s disease naturally progresses and potential drug targets”, said principal investigator Michael Rafii, M.D., assistant professor of neurosciences and interim co-director of the Alzheimer’s Disease Cooperative Study at UCSD.
Advertisement
“We’re quite excited that this could be a novel approach to treating or thinking about treating Alzheimer’s as an adjunct, as an additive therapy to the current therapies that are being developed”, commented Dr Matthew Campbell.