-
Tips for becoming a good boxer - November 6, 2020
-
7 expert tips for making your hens night a memorable one - November 6, 2020
-
5 reasons to host your Christmas party on a cruise boat - November 6, 2020
-
What to do when you’re charged with a crime - November 6, 2020
-
Should you get one or multiple dogs? Here’s all you need to know - November 3, 2020
-
A Guide: How to Build Your Very Own Magic Mirror - February 14, 2019
-
Our Top Inspirational Baseball Stars - November 24, 2018
-
Five Tech Tools That Will Help You Turn Your Blog into a Business - November 24, 2018
-
How to Indulge on Vacation without Expanding Your Waist - November 9, 2018
-
5 Strategies for Businesses to Appeal to Today’s Increasingly Mobile-Crazed Customers - November 9, 2018
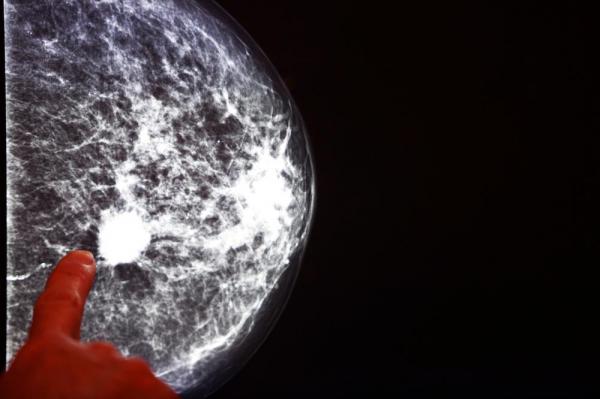
Genetic testing proves popular among women with breast cancer
The study found that 780 of the 897 women reported having undergone BRCA testing within the year following their breast cancer diagnosis.
Advertisement
The authors have found that the frequency of gene testing even increased over time. “While BRCA testing is recommended for young women with breast cancer, there has been little research into how widely these recommendations are being followed, and how concerns about genetic risk affect treatment decisions”.
Rosenberg et al. “note the need to explain the practical goal for genetic testing at the time of a new breast cancer diagnosis and address patient concerns”, write Kathleen Blazer, EdD; Thomas Slavin, MD; and Jeffrey Weitzel, MD.
He added, though, that disadvantaged American women may not have the same access to genetic testing as these largely while, well-educated, and insured women.
Jolie had both of her breasts removed in 2013 after learning she has the BRCA mutation.
But women with an underactive thyroid gland – also known as hypothyroidism – were six percent less likely to develop breast cancer, they concluded. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc. Assessing a young women’s genetic risk after a breast cancer diagnosis can have implications for subsequent treatment decisions. In 2013, the actress and filmmaker revealed her choice to have a preventative double mastectomy because she’d tested positive for the mutation.
Researchers involved with the study, published in the JAMA Oncology, analyzed data on 897 women 40 years or younger collected between 2006 and 2014 as part of the Helping Ourselves, Helping Others: Young Women’s Breast Cancer Study. Co-authors are Shari Gelber, MS, MSW, Bryce Larsen, MA, and Judy Garber, MD, MPH, of Dana-Farber; Kathryn Ruddy, MD, MPH, of the Mayo Clinic; Rulla Tamimi, ScD, of Brigham and Women’s Hospital; Lidia Schapira, MD, of Massachusetts General Hospital; Steven Come, MD, of Beth Israel Deaconess Medical Center; Virginia Borges, MD, of the University of Colorado Cancer Center.
The following year, a slightly lower percentage reported testing – 87 out of 124 women, or 70.2 per cent.
Limitations of this study included that most women would have undergone testing when Myriad Genetics was the only commercial laboratory offering clinical testing, and that testing for BRCA1 and BRCA2 was the only available option. And most of those women – 86 percent – chose to have a double-mastectomy, the study showed.
The advice stems from the fact carriers of BRCA1 and BRCA2 mutations have a higher risk of early-onset breast cancer.
“We don’t want to be doing procedures that aren’t medically indicated”, Partridge said.
And now, thanks to the ‘Angelina Jolie effect, ‘ more women than ever before are getting tested for the mutated gene. Additionally, the researchers tried to understand why some women do not get tested despite clinical recommendation.
But in reality, that counseling does not always happen, he said.
Advertisement
Among the 780 women who underwent a BRCA mutation test, 81.3% reported a negative result; 7.6% had a BRCA1 mutation, 4.5% had a BRCA2 mutation, and 4.5% had an indeterminate result or an unknown variant. And, Weitzel said, Medicaid is now paying for testing, though the coverage varies by state.