-
Tips for becoming a good boxer - November 6, 2020
-
7 expert tips for making your hens night a memorable one - November 6, 2020
-
5 reasons to host your Christmas party on a cruise boat - November 6, 2020
-
What to do when you’re charged with a crime - November 6, 2020
-
Should you get one or multiple dogs? Here’s all you need to know - November 3, 2020
-
A Guide: How to Build Your Very Own Magic Mirror - February 14, 2019
-
Our Top Inspirational Baseball Stars - November 24, 2018
-
Five Tech Tools That Will Help You Turn Your Blog into a Business - November 24, 2018
-
How to Indulge on Vacation without Expanding Your Waist - November 9, 2018
-
5 Strategies for Businesses to Appeal to Today’s Increasingly Mobile-Crazed Customers - November 9, 2018
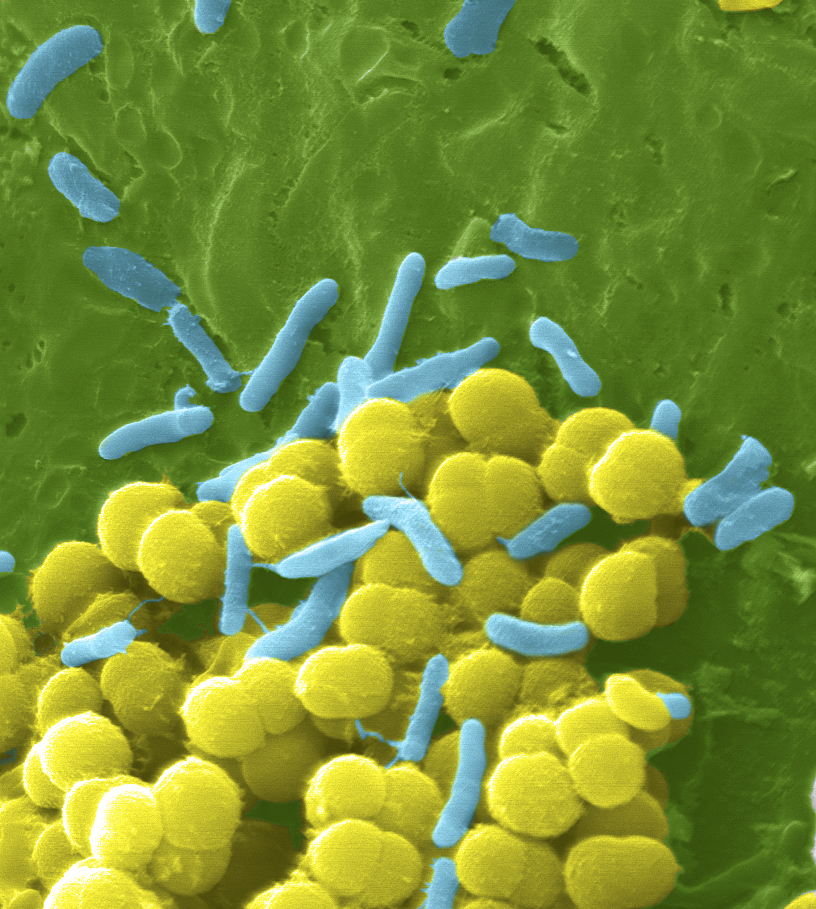
Task Force to Tackle Antimicrobial Resistance in Agriculture
Prof Davies was among a cohort of global health leaders at a summit in London discussing how the world can tackle such resistance, both in animals and humans.
Advertisement
The report suggest that these proposals would cost up to 40 billion US dollars over 10 years, which could be paid for by reallocating a fraction of funding from global institutions, allocating a small percentage of G20 nations healthcare funding, and a tax on antibiotics. “Because of the connectivity of the world and how people travel and how animals travel, unless the whole world does something we won’t solve it as a problem”, he added. The report also calls for the establishment of a Global Innovation Fund for early-stage and non-commercial research and aims to incentivise not only R&D in antibiotics but especially market entry.
His new report warns that i f antibiotics lose their effectiveness then key medical procedures – including gut surgery, caesarean sections, joint replacements, and chemotherapy – could become too risky to perform. The review was commissioned by the Government amid growing concerns about the use of the medicines in the UK.
“Our arsenal to defeat superbugs is running out and needs to be replenished”, the review said. Commissioned in 2014 by U.K. Prime Minister David Cameron and the Wellcome Trust, the report was led by economist Jim O’Neill, now the Commercial Secretary to the Treasury in the United Kingdom.
The report found that antibiotic-resistant bacteria will become a particularly big problem in developing countries and that E. coli, malaria, and tuberculosis are the biggest threats.
Ten million people could die every year from 2050 onwards unless sweeping global changes are agreed to tackle increasing resistance to antibiotics, which can turn common ailments into killers, a report warned Thursday.
World Health Organization survey results released in November 2015 suggested that 64 percent of those asked wrongly believed that penicillin-based drugs and other antibiotics can treat cold and flu, despite the fact such medicines don’t impact viruses. Failure to act will also cost the world over 100 trillion USA dollars in lost output between 2014 and 2050, the review suggests. These “market entry rewards” of around one billion United States dollars each would be given to the developers of successful new drugs, subject to certain conditions.
The 84-page report said the overuse of antibiotics should be reduced and diagnoses be improved to stop unnecessary prescriptions.
Many antibiotics that were once said to have have put an end to infectious disease are no longer working as the bugs had become resistant to them.
Lord O’Neill also proposes that doctors should be forced to perform diagnostic tests on patients before prescribing the drugs, rather than dishing them out “like sweets”.
Advertisement
Another intervention would be “to tackle the supply problem”, because “we have not seen a truly new class of antibiotics for decades”. O’Neill said pharmaceutical companies that don’t invest in research for AMR should be made to pay a charge towards the overall prevention of the resistance.