-
Tips for becoming a good boxer - November 6, 2020
-
7 expert tips for making your hens night a memorable one - November 6, 2020
-
5 reasons to host your Christmas party on a cruise boat - November 6, 2020
-
What to do when you’re charged with a crime - November 6, 2020
-
Should you get one or multiple dogs? Here’s all you need to know - November 3, 2020
-
A Guide: How to Build Your Very Own Magic Mirror - February 14, 2019
-
Our Top Inspirational Baseball Stars - November 24, 2018
-
Five Tech Tools That Will Help You Turn Your Blog into a Business - November 24, 2018
-
How to Indulge on Vacation without Expanding Your Waist - November 9, 2018
-
5 Strategies for Businesses to Appeal to Today’s Increasingly Mobile-Crazed Customers - November 9, 2018
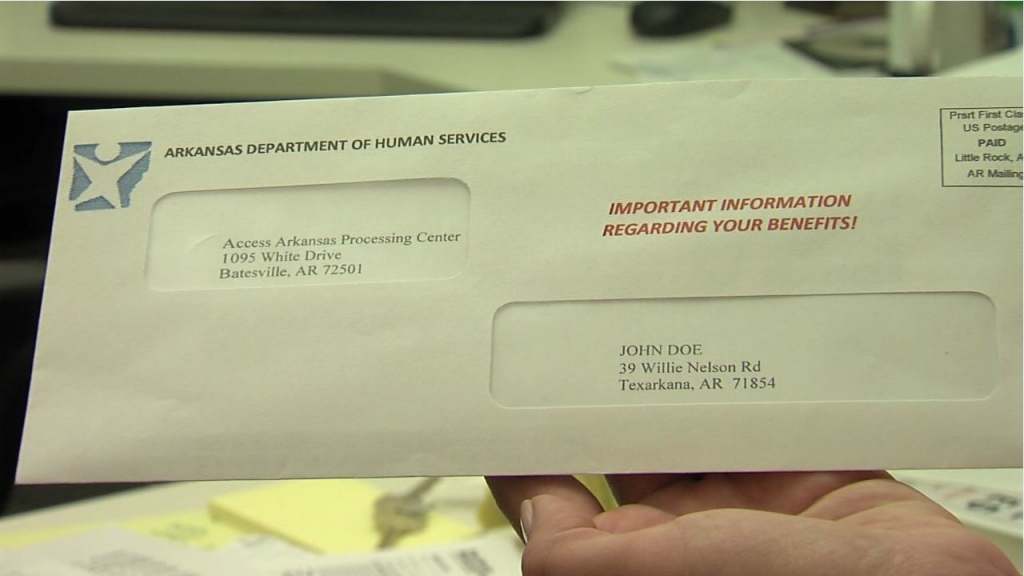
Arkansas lawmakers OK plan to tap more money for prisons
The state by the end of September will have finished redetermining eligibility for about 600,000 Medicaid and private option cases where recipients have been on the program for at least a year without an income verification.
Advertisement
On August 4, Hutchinson said he had ordered DHS to stop issuing termination notices for two weeks because the agency was experiencing an “information overload” and needed time to catch up. Another 13,000 have been sent notices that their coverage will end this month. That begins a process where nonrespondents’ benefits are terminated, with the ability to be reinstated within 90 days with all charges covered retroactively.
The Republican governor on Tuesday said the state has eliminated the backlog of responses from Medicaid recipients trying to verify their eligibility.
“I’m authorizing them to proceed today with reinstituting the verification process”. Hutchinson said in the letter and in the press conference that the 10-day window was a standard that had been set by previous administrations and that a significant percentage of respondents will not respond even if given more time. They’re sent a notice terminating coverage if they don’t respond within the 10 days or they’re found ineligible.
DHS gives people 9o days to appeal a termination of coverage, but some who lost coverage have complained that they urgently need medications.
Also announced Tuesday, two insurance companies have agreed to cover prescription drugs as the verifications continue for 30 days. QualChoice has not, he said. The 10 day income verification window was not paused while the Medicaid termination notice process was on hold.
“We’ve definitely seen improvement”, DHS spokeswoman Amy Webb said.
Advertisement
DHS didn’t have numbers on how much the backlog has eased, but said more than 300 employees have volunteered to work overtime since last Monday and it had employees working over the weekend on processing.