-
Tips for becoming a good boxer - November 6, 2020
-
7 expert tips for making your hens night a memorable one - November 6, 2020
-
5 reasons to host your Christmas party on a cruise boat - November 6, 2020
-
What to do when you’re charged with a crime - November 6, 2020
-
Should you get one or multiple dogs? Here’s all you need to know - November 3, 2020
-
A Guide: How to Build Your Very Own Magic Mirror - February 14, 2019
-
Our Top Inspirational Baseball Stars - November 24, 2018
-
Five Tech Tools That Will Help You Turn Your Blog into a Business - November 24, 2018
-
How to Indulge on Vacation without Expanding Your Waist - November 9, 2018
-
5 Strategies for Businesses to Appeal to Today’s Increasingly Mobile-Crazed Customers - November 9, 2018
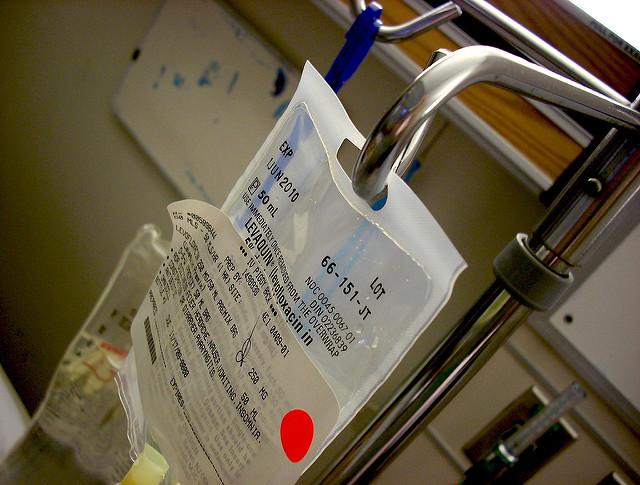
CDC: Hospital antibiotic use ‘increased significantly’
The increased use of broad-spectrum antibiotics could lead to the development of bacteria that is broadly-resistant to many class of antibiotics. The overall rate of antibiotic use for all study years was 755 days of therapy per 1,000 patient-days, a rate that also saw little change over the period of the study.
Advertisement
While the question of why doctors are increasingly turning to more powerful antibiotics was not explored in the study, the authors have some theories.
“As enrollment in the antibiotic use option grows, it will provide ongoing systematic assessment at the hospital, state, regional, and national levels”, the study authors wrote.
From 2006 up to 2012, 300 to 383 hospitals in the US for each year contributed antibiotic data to Truven Health MarketScan Hospital Drug Database (HDD) and throughout those years, 55.1% of hospitalized patients obtained at least one dose of antibiotics during hospital visit, the study reported. Data came from the Truven Health MarketScan Hospital Drug Database, which included about 300 hospitals and more than 34 million discharges. In that time, CARB launched the Antimicrobial Resistance Diagnostic Challenge, a $20 million competition to develop new diagnostic tests that healthcare providers can use to identify antibiotic-resistant bacteria, and distinguish between viral and bacterial infections. Dr. Ateev Mehrotra, associate professor at Harvard Medical School mentioned that despite knowing the side effects patients are prescribed the drugs they don’t need.
“We’ve known for decades that there are too many antibiotics being used”, Mehrotra said.
“We still give a lot of people antibiotics they don’t need”, he said.
According to Ramanan Laxminarayan, director of nonprofit Center for Disease Dynamics, Economics and Policy, because of the random use of antibiotics, it is not as effective to treat ailments as it was in the past.
“This is about the fact that doctors are human – doctors think patients want antibiotics”, Mehrotra said.
Advertisement
Other strategies suggested include feedback that compares a physician’s prescribing habits with those of peers, and order entry systems that force doctors to provide a publicly visible justification for prescribing an antibiotic. As an accompanying commentary explains, previous studies have shown that one-third of all antibiotics prescribed in outpatient settings are unnecessary, and within hospitals trends are similar.