-
Tips for becoming a good boxer - November 6, 2020
-
7 expert tips for making your hens night a memorable one - November 6, 2020
-
5 reasons to host your Christmas party on a cruise boat - November 6, 2020
-
What to do when you’re charged with a crime - November 6, 2020
-
Should you get one or multiple dogs? Here’s all you need to know - November 3, 2020
-
A Guide: How to Build Your Very Own Magic Mirror - February 14, 2019
-
Our Top Inspirational Baseball Stars - November 24, 2018
-
Five Tech Tools That Will Help You Turn Your Blog into a Business - November 24, 2018
-
How to Indulge on Vacation without Expanding Your Waist - November 9, 2018
-
5 Strategies for Businesses to Appeal to Today’s Increasingly Mobile-Crazed Customers - November 9, 2018
Aetna to cut almost 70 percent of ‘Obamacare’ footprint in 2017
Aetna’s decision to drastically reduce its participation in Affordable Care Act health insurance exchanges became the latest debating point in the race for the White House Tuesday.
Advertisement
Aetna will pull out of the 10 counties in Kentucky where it offers health insurance via the state health exchange starting in 2017. Insurers cite financial losses with marketplace plans as a factor, but financial reports show that publicly traded insurers have enjoyed robust profits in other parts of their business, including plans offered to employers or government insurance programs such as Medicare and Medicaid. “It’s new”, said Rob Field, a health care expert with Drexel University.
Competition on these exchanges will be diminished next year when three of the nations largest health insurers Aetna, UnitedHealthcare and Humana will sell individual plans in many fewer markets.
“That deterioration, and not the DOJ challenge to our Humana transaction, is ultimately what drove us to announce the narrowing of our public exchange presence for the 2017 plan year”, Crawford said.
Next year, Aetna will sell individual marketplace plans only in Delaware, Iowa, Nebraska and Virginia but none in Florida under the Aetna name or affiliated brands such as Coventry, a spokesman said.
Aetna will continue to sell coverage off the exchange.
Thats a concern in Columbia, S.C., because the Blue Cross plan does not include one of the biggest hospitals, Lexington Medical Center, and its affiliated physicians, she said.
“It’s no surprise that companies are adapting at different rates to a market where they compete for business on cost and quality rather than by denying coverage to people with preexisting conditions”, Counihan said in a statement.
“Aetna dropping out means that health insurance companies need to take a closer look at their business model and understand and accept some role as a public health provider”, he explained.
Alabama, Alaska and Oklahoma are among the states that will have one health insurer selling individual coverage on their exchanges next year.
On the surface, the reason for Aetna’s decision isn’t hard to understand. The state’s largest health insurer is seeking Goodwin’s approval to raise premium costs by an average of nearly 19 percent. They may already face dramatically increased premiums.
As it stands now, marketplace enrollees in an Aetna plan can keep their existing coverage through the end of this year, but will need to choose a new plan for 2017.
Advertisement
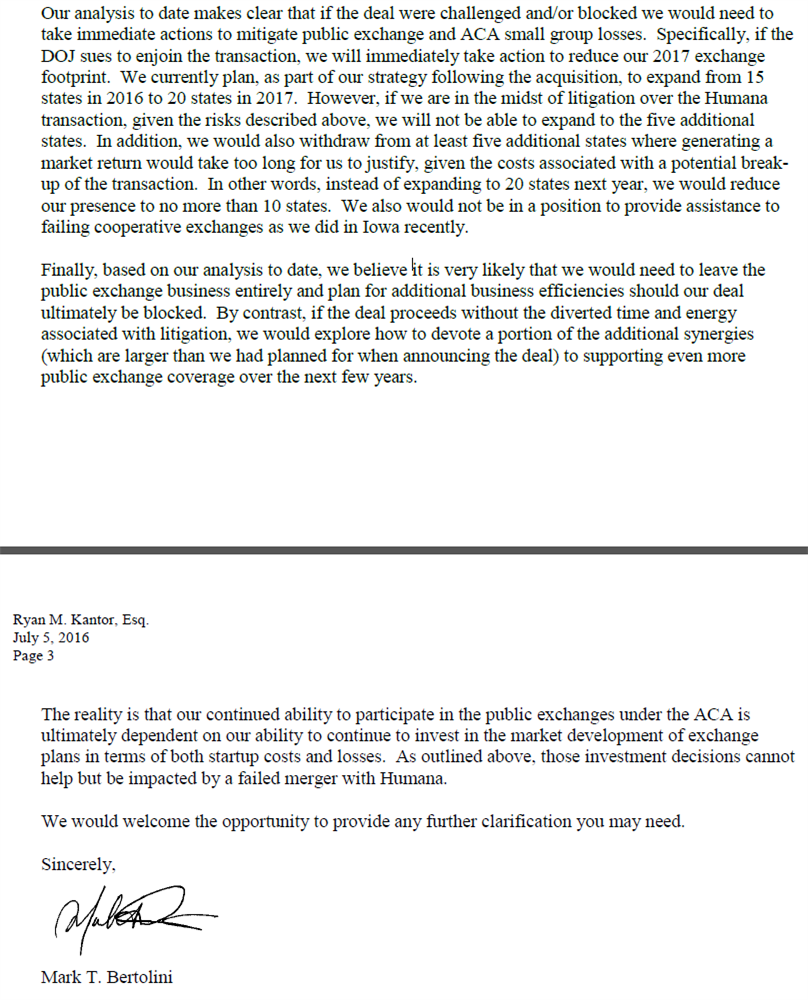
Aetna’s Bertolini, meanwhile, wrote the letter in response to the Justice Department’s query into what the likely consequences would be if it blocked the merger. Elizabeth Warren had openly speculated that Aetna’s plan to withdraw from Obamacare was retaliation for the DOJ’s suit against its merger. In the past few years, more than a dozen nonprofit insurance co-ops have shut down. Changes like eliminating taxes and finding ways to provide more affordable options could be put in place, he said.