-
Tips for becoming a good boxer - November 6, 2020
-
7 expert tips for making your hens night a memorable one - November 6, 2020
-
5 reasons to host your Christmas party on a cruise boat - November 6, 2020
-
What to do when you’re charged with a crime - November 6, 2020
-
Should you get one or multiple dogs? Here’s all you need to know - November 3, 2020
-
A Guide: How to Build Your Very Own Magic Mirror - February 14, 2019
-
Our Top Inspirational Baseball Stars - November 24, 2018
-
Five Tech Tools That Will Help You Turn Your Blog into a Business - November 24, 2018
-
How to Indulge on Vacation without Expanding Your Waist - November 9, 2018
-
5 Strategies for Businesses to Appeal to Today’s Increasingly Mobile-Crazed Customers - November 9, 2018
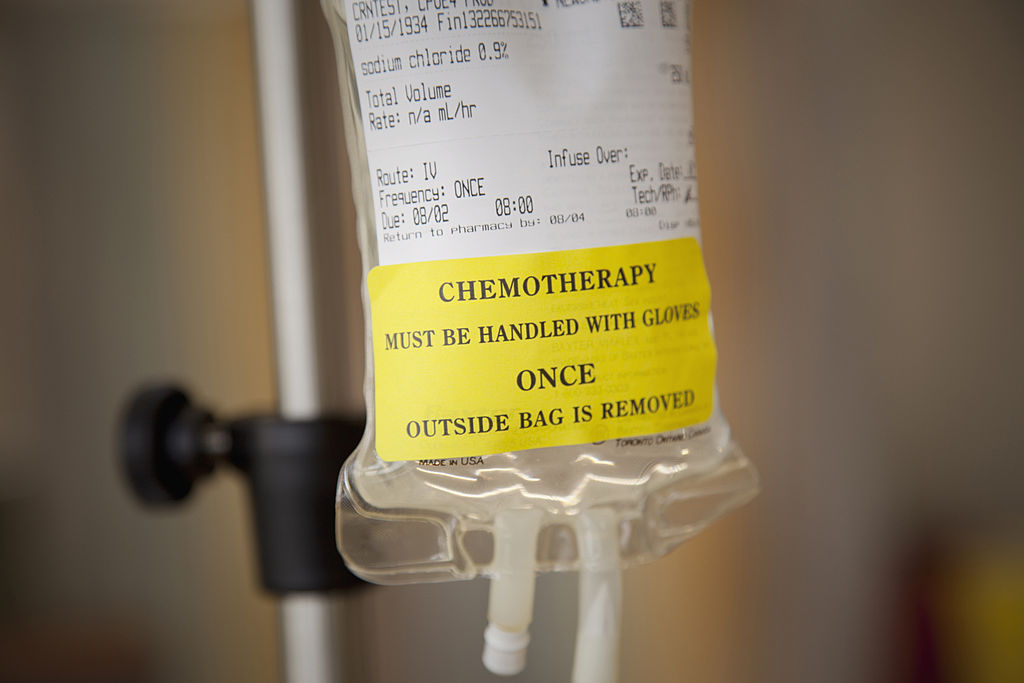
Breast cancer patients could be spared chemotherapy with a new test
In the Phase III study, researchers profiled surgically removed tumors from almost 6,700 patients using the 70-gene signature (MammaPrint) test, which classifies tumors into groups associated with a good prognosis or a poor prognosis based on the risk of distant recurrence at 5 and 10 years.
Advertisement
After five years, 94.7% of women with a high clinical risk, but low genetic risk were still alive even though they had not received chemotherapy.
All patients had received other standard therapies after their surgery including radiotherapy and hormone therapy.
By screening for 70 different markers – all of which increase the risk of the disease spreading – the MammaPrint test can accurately identify those patients who could be spared the toxic treatment.
Tamara Sandoul, Senior Policy Officer at Breast Cancer Now, said: ‘This promising test could one day help many women safely avoid overtreatment with chemotherapy.
Professor Laura van’t Veer of the University of California San Francisco, who helped design the test for Agendia, told The Telegraph: “Our ability to profile the gene expression of a tumour is transforming the way we characterise cancers and how we can more effectively treat patients”. The team also included Emiel Rutgers, MD, PhD, of the Netherlands Cancer Institute in Amsterdam, and Martine Piccart, MD, PhD, of the Université Libre de Bruxelles, in Belgium.
“Many breast cancer patients are over-treated by chemotherapy”. But a study involving early stage breast cancer shows that precision tests based on genetic fingerprints don’t take away the uncertainties. It did a thorough job of predicting which among the participants had a low risk of recurrence, according to the research.
MammaPrint searches for 70 genetic variants which make the threat of cancer returning more likely, and is considered an effective indicator of whether patients can avoid chemotherapy. However, if cancer cells were high in STC2 but low in F12, breast cancer patients only had a 10-percent chance of dying within the same period of time.
For patients facing a diagnosis of early stage breast cancer, the traditional course of treatment is typically surgery, followed by an often hard course of chemotherapy to try to make sure the cancer doesn’t recur. The researchers split these women into two groups randomly, giving one chemotherapy and withholding it from the other.
She said the 1.5 percentage-point difference in survival rates between women who got chemo and the ones who didn’t was not statistically significant, especially considering the side effects of chemo, which can include fatigue, cognitive impairment and a prolonged disruption in schedule.
This means some women could be getting chemotherapy even if it doesn’t really lower or raise their survival odds.
The researchers made use of genomic tests such as MammaPrint to obtain a woman’s genomic risk.
The study focused on women with stage 1, stage 2 and operable stage 3 breast cancer, with up to three affected lymph nodes.
RICHARD HARRIS, BYLINE: As is true for many cancers, breast cancer responds best to treatment when it is caught early before it has spread throughout the body.
Analysis of the tumor samples for the trial was performed by Agendia at no charge. An editorial accompanying the report said the study was not the final word, and current additional research would provide more clarity. In addition, van ‘t Veer holds a patent related to MammaPrint, which is licensed to Agendia NV; UCSF has no interest in the MammaPrint patent.
Advertisement
The research involved 6,693 women with early-stage breast cancer at 112 hospitals in nine European countries. A full list of authors is available in the publication.