-
Tips for becoming a good boxer - November 6, 2020
-
7 expert tips for making your hens night a memorable one - November 6, 2020
-
5 reasons to host your Christmas party on a cruise boat - November 6, 2020
-
What to do when you’re charged with a crime - November 6, 2020
-
Should you get one or multiple dogs? Here’s all you need to know - November 3, 2020
-
A Guide: How to Build Your Very Own Magic Mirror - February 14, 2019
-
Our Top Inspirational Baseball Stars - November 24, 2018
-
Five Tech Tools That Will Help You Turn Your Blog into a Business - November 24, 2018
-
How to Indulge on Vacation without Expanding Your Waist - November 9, 2018
-
5 Strategies for Businesses to Appeal to Today’s Increasingly Mobile-Crazed Customers - November 9, 2018
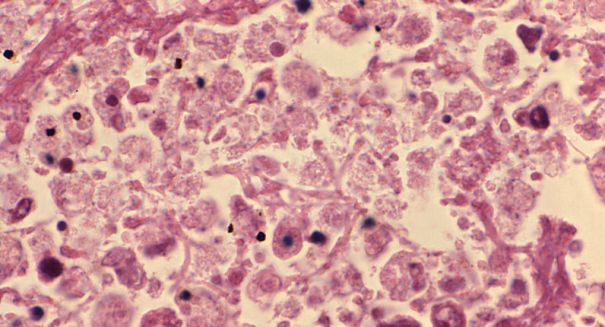
CDC: ‘Superbug’ Deaths Preventable With Better Coordination Among Healthcare
If hospitals work independently, as they do now, 31,885 people would contract CRE over 15 years in Orange County, compared with 12,614 if they worked together, according to the CDC report. “Health care facilities and public health departments need to work as a team”.
Advertisement
There are many things that can be done in order to improve the safety of health care facilities and prevent the spread of infectious diseases.
In five years, the number of infections is estimated to increase 10 percent, to 340,000 per year, according to the study, from the Centers for Disease Control and Prevention.
The team of researchers looked at the impact of four types of antibiotic-resistant bacterial infections: CRE (carbapenem-resistant Enterobacteriaceae), multi-drug resistant Pseudomonas aeruginosa, invasive MRSA(Methicillin-resistant Staphylococcus aureus), and CDIs (Clostridium difficile infections). This is especially worrisome because patients can harbor drug-resistant bacteria on their skin or in their body without showing signs or symptoms.
What’s more, coordinating efforts between hospitals would be even more effective than individual hospitals working by themselves, the study showed. These medicines can save lives when used correctly. However, they hardly communicate with each other when patients are transferred who might be infected with the antibiotic-resistant bacteria. However, antibiotics destroy the good germs that fight off the bad ones, including C. diff, putting patients at high risk for deadly diarrhea.
The report also includes computer models. They can cause pneumonia, sepsis, meningitis and other serious infections and are some of the most deadly, causing at least 2 million illnesses and killing at least 23,000 people yearly in the U.S.
Although all bacteria are slowly becoming immune to antibiotics around the world, being more judicious about when we use these treatments can also be effective in elongating antibiotic’s effectiveness on the human populace. For example, if a patient with a superbug is transferred from one hospital to another, doctors should notify the new hospital about the infection. With these in mind, Dr John Jernigan, director of the Office of HAI Prevention Research and Evaluation of the CDC’s Division of Healthcare Quality Promotion suggests hospitals, nursing homes and health authorities to “think as a community when it comes to combating antibiotic-resistant bacteria”.
In a larger picture, the food industry can use antibiotics sparingly. Bacteria have been mutating to outsmart antibiotics since the first medical antibiotic, penicillin, was mass-produced in 1944.
Advertisement
“Clearly resistance is going the wrong way”, said Jacob. “If health care facilities, nursing homes, and public health departments work together to improve antibiotic use and infection control so patients are protected”, CDC Director Tom Frieden said. He reiterated: “We are low in resources to roll (these changes) out rapidly”.