-
Tips for becoming a good boxer - November 6, 2020
-
7 expert tips for making your hens night a memorable one - November 6, 2020
-
5 reasons to host your Christmas party on a cruise boat - November 6, 2020
-
What to do when you’re charged with a crime - November 6, 2020
-
Should you get one or multiple dogs? Here’s all you need to know - November 3, 2020
-
A Guide: How to Build Your Very Own Magic Mirror - February 14, 2019
-
Our Top Inspirational Baseball Stars - November 24, 2018
-
Five Tech Tools That Will Help You Turn Your Blog into a Business - November 24, 2018
-
How to Indulge on Vacation without Expanding Your Waist - November 9, 2018
-
5 Strategies for Businesses to Appeal to Today’s Increasingly Mobile-Crazed Customers - November 9, 2018
Cell Therapy Puts Advanced Lymphoma into Remission
Of the remaining 12 patients who received different chemotherapy, only one went into complete remission after auto T-cell infusion. 50 percent of the 18 patients who were evaluable for efficacy after receiving vehicle T cells and chemotherapy agents fludarabine and cyclophosphamide (Cy/Flu) had a complete response, which compares favorably to the 8 percent complete response rate in patients who received JCAR014 plus cyclophosphamide-based chemotherapy without fludarabine.
Advertisement
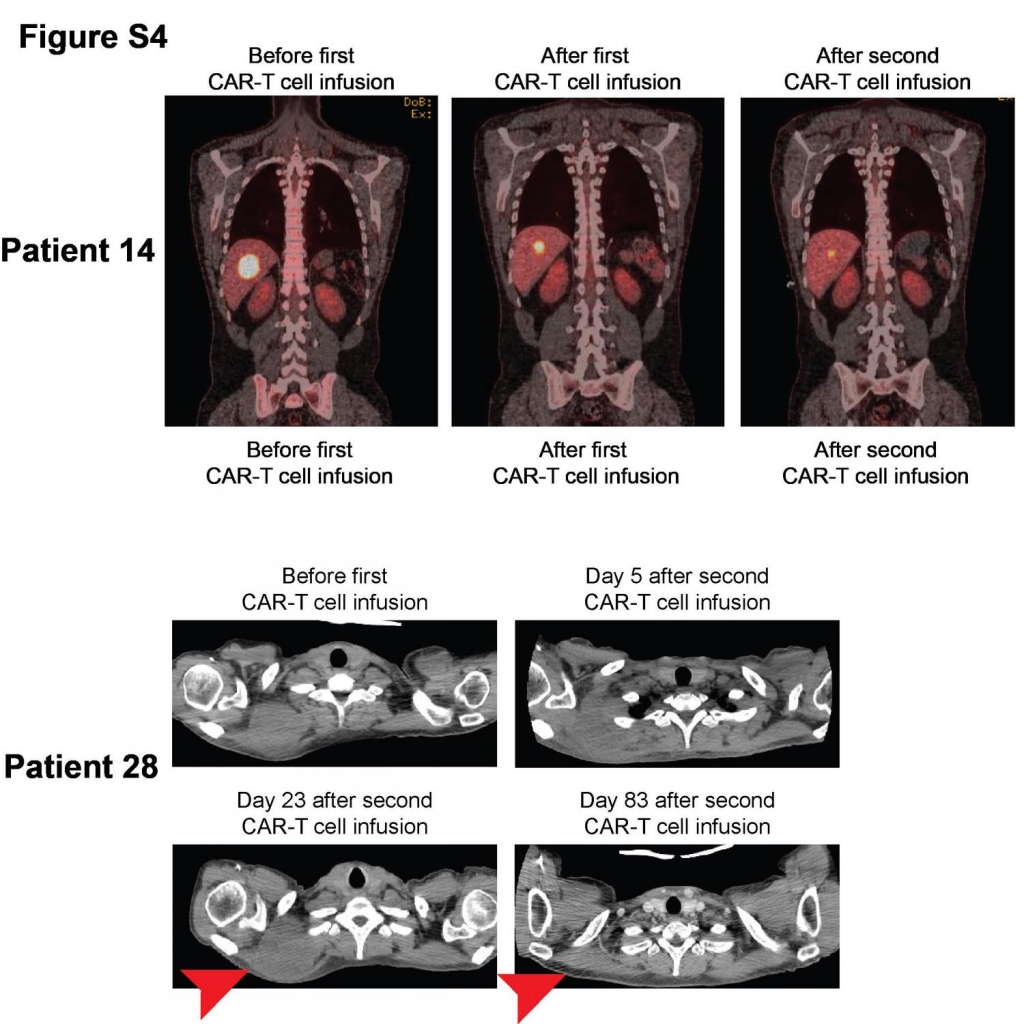
“This is important because it will help guide the design of future trials using these specialised T cells”. Imaging studies from Patients 14 and 28, who received Cy/Fly lymphodepletion before their first cycle of CAR-T cells, demonstrate tumor regression after a second cycle of Cy/Flu lymphodepletion chemotherapy and CAR-T cell infusion at an equivalent or higher dose of CAR-T cells.
JCAR014’s hallmark is its use of a one-to-one ratio of helper (CD4+) and killer (CD8+) auto T cells, which join forces to kill tumor cells that produce CD19, a molecule found on the surface of many blood cancer cells, including lymphoma and leukemia.
In a paper published today in Science Translational Medicine, researchers from Fred Hutchinson Cancer Research Center shared data from an early-phase study of patients with advanced non-Hodgkin lymphoma (NHL) who received JCAR014, a Chimeric Antigen Receptor (CAR) T cell treatment, and chemotherapy. Patients receive chemotherapy to deplete the number of cancerous B-cells and other immune cells in the body, which helps the genetically modified T-cells multiply more and survive longer.
In this experimental therapy, white blood cells known as T-cells are removed from the patient’s bloodstream.
“Like JCAR014, JCAR017 uses a one-to-one ratio of helper and killer vehicle T cells, and the company believes it has the potential to be a “best-in-class” treatment for non-Hodgkin lymphoma, chronic lymphocytic leukemia, and adult and pediatric acute lymphoblastic leukemia”, Juno said in a statement.
An experimental therapy known as immunotherapy has shown promise in treating patients with non-Hodgkin lymphoma, a blood cancer that affects the lymph system, United States researchers said Wednesday. “And then by adjusting the dose, we could improve what we call the therapeutic index: the benefit against the tumor, without too much toxicity”.
“They really had very few treatment options at the time they enrolled in our study”, Riddell said.
The approach involves removing specialised immune cells, called T cells, from a patient and engineering them so that they recognise and kill cancer cells when reintroduced into the patient.
After reengineering, the cells were multiplied in the lab using a process unique to Fred Hutch, in which cells undergo an extra growth-stimulating step. There, the cells encountered their CD19 targets, began to multiply, and went to work.
The addition of a second chemo drug in the lymphodepletion step helped the auto T cells multiply more and survive longer in these patients than in those who had received one type of chemo, the researchers found. This included fewer side effects and improved responses.
The findings suggest that perfecting the combination of chemotherapy and immune cells is vital to unlocking the full potential of CAR-T cell therapies. Seven of these participants, or 64 percent, went into complete remission. Turtle suspects that the fact that leukemia flows as a liquid in the blood and marrow makes it easier for the auto T-cells to attack that cancer.
Novartis’ decision to scale back on its CAR-T research has grabbed the headlines in recent months, but biotech Juno, itself the subject of major headlines over the summer when safety concerns briefly halted one its studies, is looking to its recent data as a positive for the field. “And that may relate to the fact that lymphoma often grows as lumps, so it may be a more-complex tumor microenvironment”.
Advertisement
The factors in lymphoma tumors that may impede T-cell activity ― and ways to circumvent them ― still need to be pinpointed, Turtle said.