-
Tips for becoming a good boxer - November 6, 2020
-
7 expert tips for making your hens night a memorable one - November 6, 2020
-
5 reasons to host your Christmas party on a cruise boat - November 6, 2020
-
What to do when you’re charged with a crime - November 6, 2020
-
Should you get one or multiple dogs? Here’s all you need to know - November 3, 2020
-
A Guide: How to Build Your Very Own Magic Mirror - February 14, 2019
-
Our Top Inspirational Baseball Stars - November 24, 2018
-
Five Tech Tools That Will Help You Turn Your Blog into a Business - November 24, 2018
-
How to Indulge on Vacation without Expanding Your Waist - November 9, 2018
-
5 Strategies for Businesses to Appeal to Today’s Increasingly Mobile-Crazed Customers - November 9, 2018
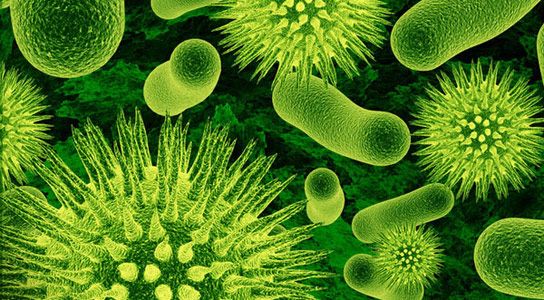
Healthcare coordination could fight ‘superbug’ infections in US
That is unless coordination improves among facilities within the country’s public health care system and Congress provides the funds for those reforms to combat the deadly microbes.
Advertisement
In five years, the number of infections is estimated to increase 10 percent, to 340,000 per year, according to the study, from the Centers for Disease Control and Prevention. “Optimizing implementation of basic infection control practice within individual facilities will be of fundamental importance to this effort”, CDC said. The public health institute is calling the coordination of hospitals, nursing homes and health authorities to prevent the threats of the infections in the coming years. “Incorporating such coordinated approaches at a national level could help ensure such actions are effective”.
There were at least 310,000 cases of multidrug-resistant bacteria in the US last 2011 that can commonly be found from hospitals: Pseudomonas aeruginosa, carbapenem-resistant Enterobacteriaceae (CRE), Clostridium difficile which can cause awful diarrhea (patients who take antibiotics can have higher tendency to acquire this type of infection) and invasive methicillin-resistant Staphylococcus aureus (MRSA). But when doctors overprescribe them, incorrectly use them to treat viruses, or when patients don’t finish the entire course, the treatment can backfire as bacteria adapt and become resistant to antibiotics.
In order to turn the data into action that prevents illness and saves lives the authors of the report urged public health departments to track and alert healthcare facilities of antibiotic-resistant bacteria outbreaks in their area and other facilities.
So far, “independent, institution-based efforts to prevent transmission have been inadequate”, the researchers wrote in the study, published this week in the CDC journal Morbidity and Mortality Weekly Report.
The health care industry is well aware of the spread of powerful germs between different hospitals and nursing homes. The CDC report says this self-reliant approach isn’t working, and patients are getting sick and dying as a result. Every year in the United States, about 2 million illnesses and 23,000 deaths result from superbug infections, according to the CDC. This is especially worrisome because patients can harbor drug-resistant bacteria on their skin or in their body without showing signs or symptoms. For example, if a patient with a superbug is transferred from one hospital to another, doctors should notify the new hospital about the infection. The Obama Administration, started with the White House itself, has already decreed the use of antibiotics to be seized over their food service.
Advertisement
“No one facility can stop this, because outbreaks move across facilities”, said CDC Director Dr. Tom Frieden.