-
Tips for becoming a good boxer - November 6, 2020
-
7 expert tips for making your hens night a memorable one - November 6, 2020
-
5 reasons to host your Christmas party on a cruise boat - November 6, 2020
-
What to do when you’re charged with a crime - November 6, 2020
-
Should you get one or multiple dogs? Here’s all you need to know - November 3, 2020
-
A Guide: How to Build Your Very Own Magic Mirror - February 14, 2019
-
Our Top Inspirational Baseball Stars - November 24, 2018
-
Five Tech Tools That Will Help You Turn Your Blog into a Business - November 24, 2018
-
How to Indulge on Vacation without Expanding Your Waist - November 9, 2018
-
5 Strategies for Businesses to Appeal to Today’s Increasingly Mobile-Crazed Customers - November 9, 2018
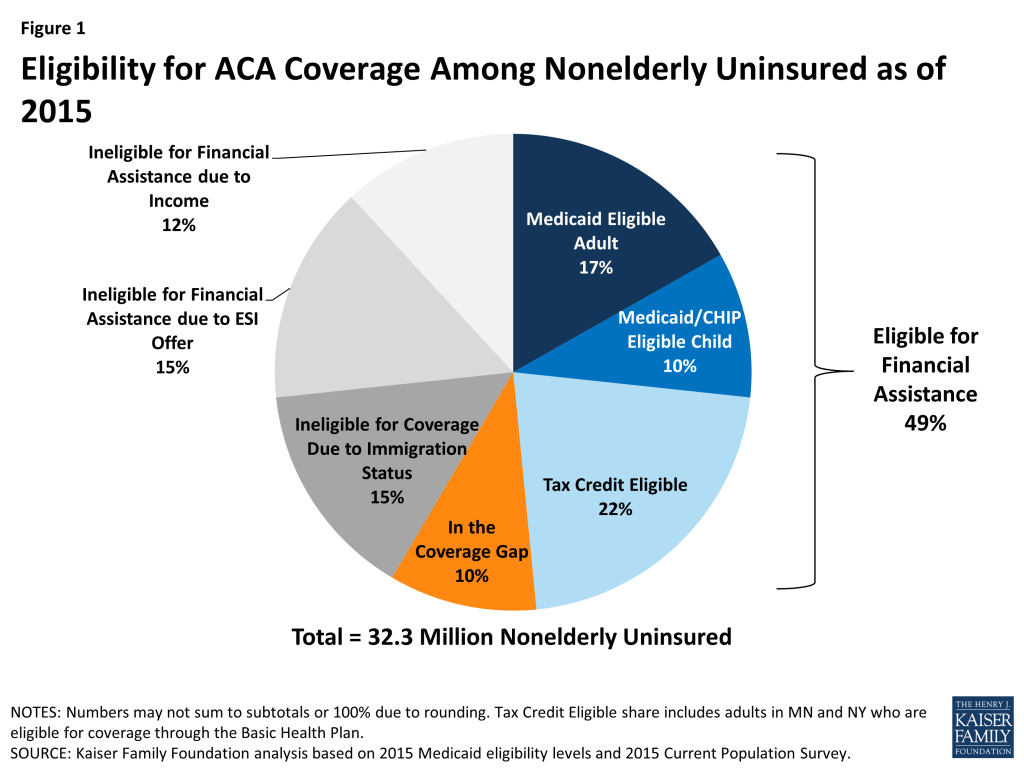
More than half of uninsured are eligible for financial help
Others have enough income to buy it on their own or through their employer, but don’t. In Nebraska, just 35 percent of the uninsured population are eligible for assistance, while 75 percent of the uninsured in West Virginia qualify. But experts broadly acknowledge that the remaining uninsured are the hardest population to reach, since they have resisted buying coverage or are unaware of the opportunity to buy it over the two enrollment periods.
Advertisement
“We applaud HealthCare.gov’s decision to support “Do Not Track” and give their users strong privacy controls”, said Cooper Quintin, a staff technologist with the foundation.
· Qualify for subsidized Marketplace plans but haven’t enrolled, 825,000 (30%).
· Could enroll in an employer-sponsored plan but have not, 417,000 (15%). And 384,000 did not qualify because they could not prove their citizenship.
The percentage is lower in Texas, among other reasons, because state GOP leaders have rejected Medicaid expansion and the state has a disproportionate number of illegal immigrants, who are shut out of virtually all government programs assisting people with health insurance.
· Remain uninsured even though they have substantial incomes, too high to qualify for tax credits on the Marketplace, 290,000 (10%).
About 703,000 Floridians were ineligible for federal law’s tax credits because they earn too much or were offered coverage through work (whether it was affordable or not).
Florida and four other states account for 40 percent of the nation’s uninsured who could receive tax credits or Medicaid benefits.
As of the beginning of 2015, 32.3 million nonelderly people lacked health coverage in the U.S. Nationally, we estimate that almost half (15.7 million, or 49%) of this population is eligible for financial assistance to gain coverage through either Medicaid or subsidized Marketplace coverage (Figure 1).
Basically, “gappers” earn too much to qualify for Medicaid.
The research team’s finding that there are more than 300,000 more Medicaid eligible will not be good news for Florida lawmakers.
The statewide managed care program that Medicaid launched in 2013 and 2014 has trimmed the per-enrollee cost, the economic report says.
They were confused about premium payment requirements.
As The New York Times reports, there is no comprehensive data on why people drop or lose their marketplace coverage.
The Affordable Care Act has transformed the healthcare industry, with its provisions having led to massive changes in the way that millions of Americans get their healthcare needs met. Amid all the controversy surrounding the legislation, it’s easy to forget that the stated goal of Obamacare was to reduce the percentage of people lacking health insurance. Those who are Medicaid eligible include people who were previously eligible as well as those newly eligible under the ACA.
The remainder of the uninsured either has an offer of ESI (4.9 million, or 15%) or has an income above the limit for premium tax credits but could purchase unsubsidized Marketplace coverage (3.7 million, or 12%). Texas is one of seven states that also exclude adults who are legal immigrants from Medicaid, the state-federal program for the poor.
Advertisement
Carol Gentry is a special correspondent for WUSF in Tampa.