-
Tips for becoming a good boxer - November 6, 2020
-
7 expert tips for making your hens night a memorable one - November 6, 2020
-
5 reasons to host your Christmas party on a cruise boat - November 6, 2020
-
What to do when you’re charged with a crime - November 6, 2020
-
Should you get one or multiple dogs? Here’s all you need to know - November 3, 2020
-
A Guide: How to Build Your Very Own Magic Mirror - February 14, 2019
-
Our Top Inspirational Baseball Stars - November 24, 2018
-
Five Tech Tools That Will Help You Turn Your Blog into a Business - November 24, 2018
-
How to Indulge on Vacation without Expanding Your Waist - November 9, 2018
-
5 Strategies for Businesses to Appeal to Today’s Increasingly Mobile-Crazed Customers - November 9, 2018
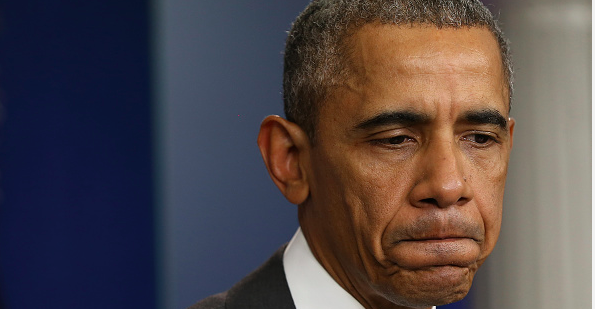
UnitedHealth says losses may force it out of Obamacare exchanges
The financial assistance depends on income, however, and particularly for people making more than 250 percent of the poverty line, coverage can seem extremely expensive – especially for those who remember the cut-rate coverage available before the Affordable Care Act, when insurers could sell policies with skimpier benefits and screen for pre-existing conditions.
Advertisement
He added that the plans on the exchanges haven’t been profitable because the enrollees are utilizing services at greater-than-expected rates, including healthy people who have “no disincentive to over-use the plans”. But such is not the case with Kaiser Permanente, which announced Thursday that it remains committed to continue participating in the health exchanges. The small health insurer, which focuses on Medicaid, also said its exchange business was performing in line with its expectations. Blue Cross also stopped offering on the individual market its PPO plan that featured its broadest provider network. “They hope it will be at a few point, but it’s not there yet, and without a public option [a government-sponsored health plan] and with the co-ops exiting in much of the country, you know Obamacare needs private insurers to play”.
The Obama administration has said itaims to have about 10 million peoplewith paid-up coverage on the state and federal health-law exchanges by the end of 2016.
The S&P 500’s health-care sector fell 1.6% after UnitedHealth told investors it expected heavy losses from the Obamacare exchanges and would consider withdrawing from them; UNH ended -5.6%, while Aetna, Anthem and Cigna all fell more than 5%. The company now expects 2015 earnings of about $6 per share, down from its previous forecast for $6.25 to $6.35 per share.
“I don’t think it’s a disaster”, he said, noting that the insurer largely stayed out of the market in the first year and has come out of the exchanges in several states last year. The company also suggested that it would expand into 11 more exchanges next year. The company has yet to make a decision about its exit from the public exchanges.
UnitedHealth Group said last month it expects better results from its ACA policies sold in more than two dozen states in 2016. “Today’s statement by one issuer is not indicative of the Marketplace’s strength and viability”.
UnitedHealth shares sank more than 5 percent, or $6.31, to $111 in premarket trading Thursday. This is the largest insurer in the nation saying it will lose more and more money selling the kinds of plans Obamacare requires to be sold on the exchange.
“The reality is we continue to see more people signing up for health insurance and more issuers entering the marketplaces”, Ben Wakana, a spokesman for the Department of Health and Human Services, said in an e-mail.
That has been one of the complaints recently by Blue Cross and Blue Shield of Louisiana. “There’s probably more going than coming, but it’s not the end of the game yet”, he said.
UnitedHealth’s latest move reflects “a continuing deteriora tion” in claims and “tempered” expectations for 2016 enrollment. The ACA has delivered more transparency to the health care market, more choice for consumers, and has barred insurers from denying insurance coverage to patients, he said. It had about 815,000 members in plans on the exchanges and 275,000 in plans sold off the exchanges.
Insurers expected challenges as they built this business over the past few years. But that the pool is experiencing adverse selection over the course of the year, as healthy people stop paying their premiums, and sicker people buy in.
Advertisement
Leemore Dafny at Northwestern’s Kellogg School of Management said just because UnitedHealth took a hit doesn’t mean all insurers will take a bath.