-
Tips for becoming a good boxer - November 6, 2020
-
7 expert tips for making your hens night a memorable one - November 6, 2020
-
5 reasons to host your Christmas party on a cruise boat - November 6, 2020
-
What to do when you’re charged with a crime - November 6, 2020
-
Should you get one or multiple dogs? Here’s all you need to know - November 3, 2020
-
A Guide: How to Build Your Very Own Magic Mirror - February 14, 2019
-
Our Top Inspirational Baseball Stars - November 24, 2018
-
Five Tech Tools That Will Help You Turn Your Blog into a Business - November 24, 2018
-
How to Indulge on Vacation without Expanding Your Waist - November 9, 2018
-
5 Strategies for Businesses to Appeal to Today’s Increasingly Mobile-Crazed Customers - November 9, 2018
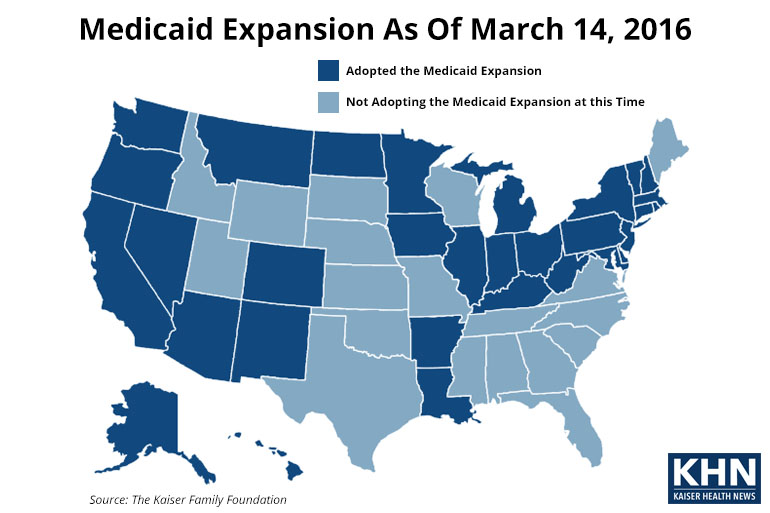
UnitedHealth to trim ACA exchanges to ‘handful’ of states
Overall, the Affordable Care Act has resulted in about 20 million newly insured adults, according to the administration’s estimate. But a spokesman confirmed Nevada and Virginia would be among the states where it will retain a presence. About 300,000 Virginians are covered by these policies. And the plan I had previous year was unceremoniously dropped.
Advertisement
“The industry is clearly setting the stage for bigger premium increases in 2017”, said Larry Levitt of the Kaiser Family Foundation. “While United is generally not a low premium insurer, there are markets where it offers one of the two lowest cost plans, and an exit could increase benchmark premiums”. Either they need to get approval from state regulators for another round of large premium increases, or they may bail out altogether.
First, go back and read my Monday Obamacare post, which enumerated the latest headaches and failures associated with the Obama administration’s unpopular, failing healthcare overhaul.
Diagnoses of diabetes and high cholesterol each rose more than 5 percentage points.
UnitedHealth has already made a decision to pull out of Arkansas, Georgia and MI in 2017, and Hemsley told analysts during a Tuesday morning conference call that his company does not want to take the financial risk from the exchanges into 2017. “State exchanges will have some fluctuation, but AHCT will continue to meet the needs of CT residents”. But insurers have struggled with higher than expected claims from that business.
A separate program that limits any losses also ends this year.
The vast majority of the country’s 11 million unauthorized immigrants, about 70 percent of whom are Hispanic, still lack coverage, said Mark Hugo Lopez, director of Hispanic research at the Pew Research Center.
United officials said they were unwilling to keep losing money. Insurers have been pounding the drum about problems with ObamaCare pricing. The company also raised its forecast for 2016.
Part of the challenge is that insurers’ rates must meet two key tests.
“It’s likely that in places where they were one of the only insurance companies, and they priced low relative to their competitors, they’re important players”, Cynthia Cox, one of the report’s authors, said by phone.
That includes cooks and waitresses, cashiers and hairdressers – the kind of low-paying and often part-time workers who couldn’t afford insurance premiums. “That data shows that the future of the marketplace remains strong”.
“For Tax Year 2015, many employers were scrambling to push out year-end IRS forms without having methodically prepared all along for the compliance, or noncompliance, measures they were reporting on those forms”, Doolin said.
The analysis is based on insurer participation and premiums in marketplaces in 2016. Analysts had estimated adjusted earnings of $7.73 on average. Costs for 2016 were set to rise 6 percent to 8 percent nationwide, insurance experts say. They found no improvement in self-reported health among low-income adults in the expansion states.
“The increased detection of chronic health conditions under the Medicaid expansions could have important implications for both population health and national health care spending if it leads to improved management and control of these conditions”, noted the study.
“These rate requests are subject to review by the Bureau of Insurance”, Whorley said.
Advertisement
Ress can be reached by phone at 757 247 4535.