-
Tips for becoming a good boxer - November 6, 2020
-
7 expert tips for making your hens night a memorable one - November 6, 2020
-
5 reasons to host your Christmas party on a cruise boat - November 6, 2020
-
What to do when you’re charged with a crime - November 6, 2020
-
Should you get one or multiple dogs? Here’s all you need to know - November 3, 2020
-
A Guide: How to Build Your Very Own Magic Mirror - February 14, 2019
-
Our Top Inspirational Baseball Stars - November 24, 2018
-
Five Tech Tools That Will Help You Turn Your Blog into a Business - November 24, 2018
-
How to Indulge on Vacation without Expanding Your Waist - November 9, 2018
-
5 Strategies for Businesses to Appeal to Today’s Increasingly Mobile-Crazed Customers - November 9, 2018
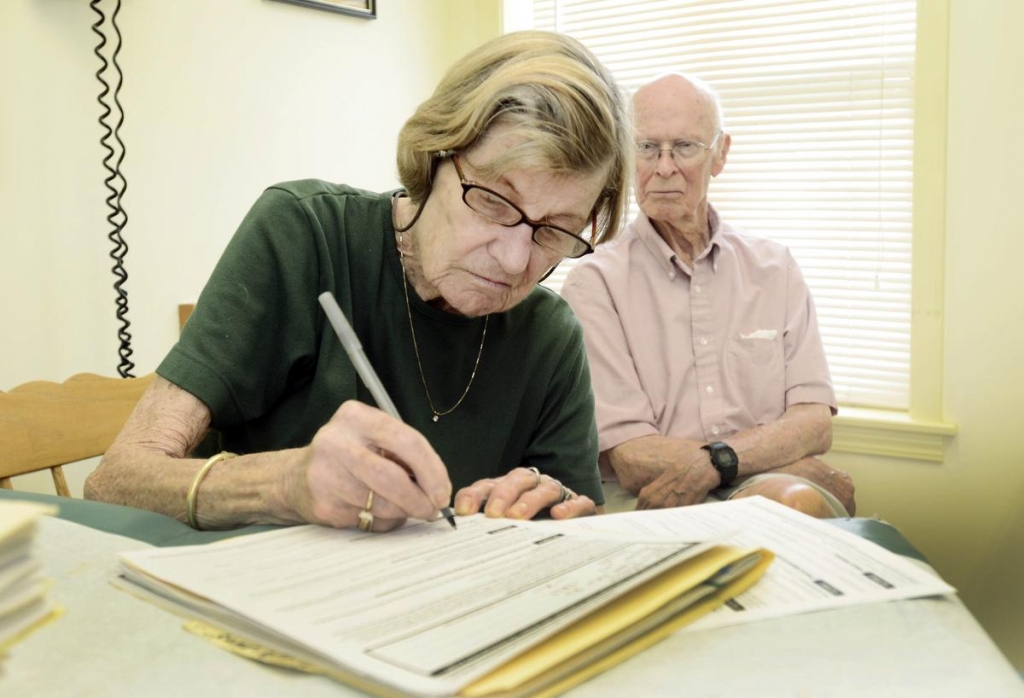
US’ Medicare to cover end-of-life counseling
WASHINGTON – Medicare said Wednesday it plans to pay doctors to counsel patients about end-of-life care, the same idea that sparked accusations of “death panels” and fanned a political furor around President Barack Obama’s health care law six years ago.
Advertisement
“This proposal, if finalized, will help our patients and their families, who often look to us for assistance with planning for their future care”, said Steven R. Counsell, MD, AGSF, President of the AGS. However, this did not translate into an increase in the use of living wills, which fell from 49% to 40%, or an increase in end-of-life discussions, which also fell from 68% to 60% in the same period.
Palin was later quoted as saying the nature of the conversations with health care providers after a patient’s health changes significantly can be coercive, especially when part of the bill’s intent is to reduce the growth of health care spending.
Medicare, the federal program that insures 55 million older and disabled Americans, announced plans on Wednesday to reimburse doctors for conversations with patients about whether and how they would want to be kept alive if they became too sick to speak for themselves.
Julie Rovner, senior correspondent with Kaiser Health News, tells our Newscast unit that many medical groups, including the American Medical Association, have long recommended the move.
End-of-life discussions shouldn’t be regarded as taboo.
Proponents-which includes most provider organizations-say advanced care planning both lowers systemic costs and provides higher patient satisfaction and better care.
Many doctors have said they regard such counseling as a common-sense option, and some already have such conversations with their patients without billing extra.
The agency is soliciting feedback on whether to expand the Comprehensive Primary Care Initiative and how to reimburse care consultations between primary-care docs and specialists that require “extensive discussion, information-sharing and planning”. Opponents declared the conversations a step toward “death panels” that would have the government ration care for the elderly and infirm. Mack, the lead author, said decisions about treating teens and young adults are challenging because they are at a different stage of life; some may have young children and want to extend life as long as possible.
“We feel there is pervasive bias against treatment that is occurring in advance care planning that involves nudging individuals to reject lifesaving medical treatment”, he said. The National Academy of Medicine (formerly the Institute of Medicine) is one of many medical research bodies that have examined the issue. “In addition, we seek comment on whether payment for advance care planning is appropriate in other circumstances such as an optional element, at the beneficiary’s discretion, of the annual wellness visit”.
Balch said his organization was trying to find a congressional sponsor for a bill that would instead direct Medicare to produce materials about end-of-life decisions that reflect a range of views, including those “concerned with protecting people’s right to treatment”.
Advertisement
“Patients and their families should be encouraged to think about how they want to be treated at the end of their life and to express their goals, values, and preferences to their physicians”.