-
Tips for becoming a good boxer - November 6, 2020
-
7 expert tips for making your hens night a memorable one - November 6, 2020
-
5 reasons to host your Christmas party on a cruise boat - November 6, 2020
-
What to do when you’re charged with a crime - November 6, 2020
-
Should you get one or multiple dogs? Here’s all you need to know - November 3, 2020
-
A Guide: How to Build Your Very Own Magic Mirror - February 14, 2019
-
Our Top Inspirational Baseball Stars - November 24, 2018
-
Five Tech Tools That Will Help You Turn Your Blog into a Business - November 24, 2018
-
How to Indulge on Vacation without Expanding Your Waist - November 9, 2018
-
5 Strategies for Businesses to Appeal to Today’s Increasingly Mobile-Crazed Customers - November 9, 2018
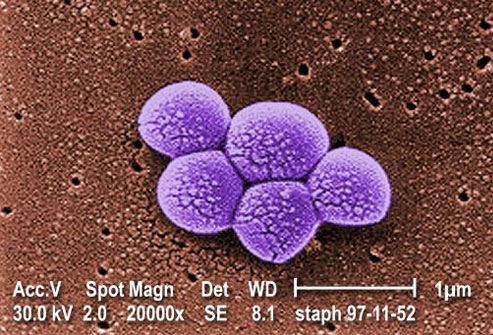
Wrong antibiotic ‘can make superbug worse’
Since MRSA takes a couple of days to culture, early diagnosis can be hard and in the meantime a beta-lactam antibiotic may have been prescribed as an empiric treatment. The findings could have important clinical implications, say the scientists writing in the journal Cell Host & Microbe.
Advertisement
The new research by Dr. Liu and colleagues is based on laboratory studies of mice that found rodents treated with antibiotics similar to methicillin, called beta lactams, caused the MRSA bacteria to build cell walls that are highly inflammatory and damaging to tissues.
Medical professionals also know that when beginning treatment there is a risk of the patient getting worse before they begin to show improvement due to the release of endotoxins by bacteria, which can cause septicemia (blood poisoning), organ failure and death. A new study suggests that treatment with the wrong antibiotic could make MRSA-induced infections worse. The next step will be to obtain human data.
“Individuals infected with MRSA who receive a beta-lactam antibiotic-one of the most common types of antibiotics-could end up being sicker than if they received no treatment at all”, says co-senior study author George Liu of Cedars-Sinai Medical Center. He added that their findings underscore the urgent requirement to make awareness of MRSA better along with diagnosing these infections faster to avoid prescribing antibiotics that could put patients’ lives at risk.
Staphylococcus aureus, also termed as “staph”, is a kind of bacteria usually carried on the skin or inside the nose of healthy people. About one-third of the population is colonized with staph, but approximately 1% is colonized with MRSA, which is resistant to methicillin and many other antibiotics.
MRSA causes 80,000 invasive infections and 11,000 related deaths per year in the United States, according to 2011 figures from the Centers for Disease Control and Prevention. Apparently, beta-lactam antibiotic’s mechanism of action involves neutralizing the enzymes in bacteria that make cell walls. This enables the MRSA superbug to continue making its cell wall, which has a different structure to normal staph.
Now, this study is still relatively new so the results definitely require more research. A high percentage of hospital-acquired infections are caused by highly resistant bacteria such as methicillin-resistant Staphylococcus aureus (MRSA) or multidrug-resistant Gram-negative bacteria.
“We now have evidence that the very factor that defines certain S. aureus as MRSA is a factor that can also make MRSA more pathogenic”, study author Sabrina Muller of Cedars-Sinai Medical Center said reported in the press release. However when MRSA is exposed to beta-lactams, rather than destroying the cell wall it causes an enzyme called PBP2A to be rendered inactive and alters the cell wall allowing the MRSA not only to proliferate but inducing a powerful inflammatory reaction.
MRSA infections were made worse by antibiotics in mice that were part of the latest study.
Advertisement
The researchers first examined the structural makeup of MRSA and found that unlike normal S. aureus, MRSA can bypass the effects of beta-lactam antibiotics.